When pain strikes your back or neck, it’s natural to want answers. Many patients ask us whether they should have an MRI or X-ray before starting treatment, believing that a scan will reveal exactly what’s wrong.
At Costa Health, we spend considerable time explaining when scans are genuinely helpful, when they’re not, and why imaging is often not the first step for most people with musculoskeletal pain. Understanding this can reduce unnecessary worry and help ensure your treatment targets the true cause of your symptoms.
Why People Often Think They Need a Scan
Pain can feel alarming, particularly when it affects the back or neck, or radiates into another area such as the hip or knee. Many people worry there may be serious damage causing their pain, and scans are often seen as the way to ‘see what’s wrong’.
It’s also common to assume that more information automatically leads to better treatment. However, this is not always the case with musculoskeletal conditions.
When Scans Are Genuinely Helpful
Scans can be important in specific situations, including:
- Significant trauma such as a fall or accident
- Progressive neurological symptoms like increasing weakness or numbness
- Loss of coordination or changes in bladder or bowel function
- When serious underlying conditions need to be ruled out
In these situations, imaging helps guide appropriate medical care and is an essential part of the diagnostic process.
When Scans Are Often Not Needed
For most back, neck, hip, or knee pain related to movement, sport, posture, or daily activities, scans are not routinely required.
Research consistently shows that many findings on scans do not correlate well with pain. Disc bulges, disc herniations, and degenerative changes are commonly seen in people who have no symptoms at all.
Quick Tip: If your pain came on gradually without trauma and you have no neurological symptoms, a thorough clinical assessment is usually more valuable than rushing to get a scan.
Why Scan Results Can Be Misleading
Seeing changes on a scan can sometimes increase fear and lead people to believe they are damaged, even when those findings are not the source of their pain.
This can result in unnecessary avoidance of movement, which may actually slow recovery. The medical literature refers to this as ‘nocebo effect’, where the expectation of a negative outcome contributes to poorer results.
A Clinical Case Example
We often see this in practice. A runner recently attended the clinic with pain on the outside of the thigh travelling down towards the knee.
A scan had previously shown a disc prolapse in the lower back, and the patient understandably believed this was causing their symptoms.
However, a detailed clinical assessment told a different story. Movement testing, strength assessment, and analysis of running mechanics identified overload of the lateral muscles around the pelvis. This overload was altering hip control and placing increased strain on the structures around the knee.
In this case, the disc prolapse seen on the scan was an incidental finding rather than the cause of symptoms. This is not uncommon. Disc herniations are frequently visible on scans in people who have no pain at all.
Why Clinical Assessment Is Essential
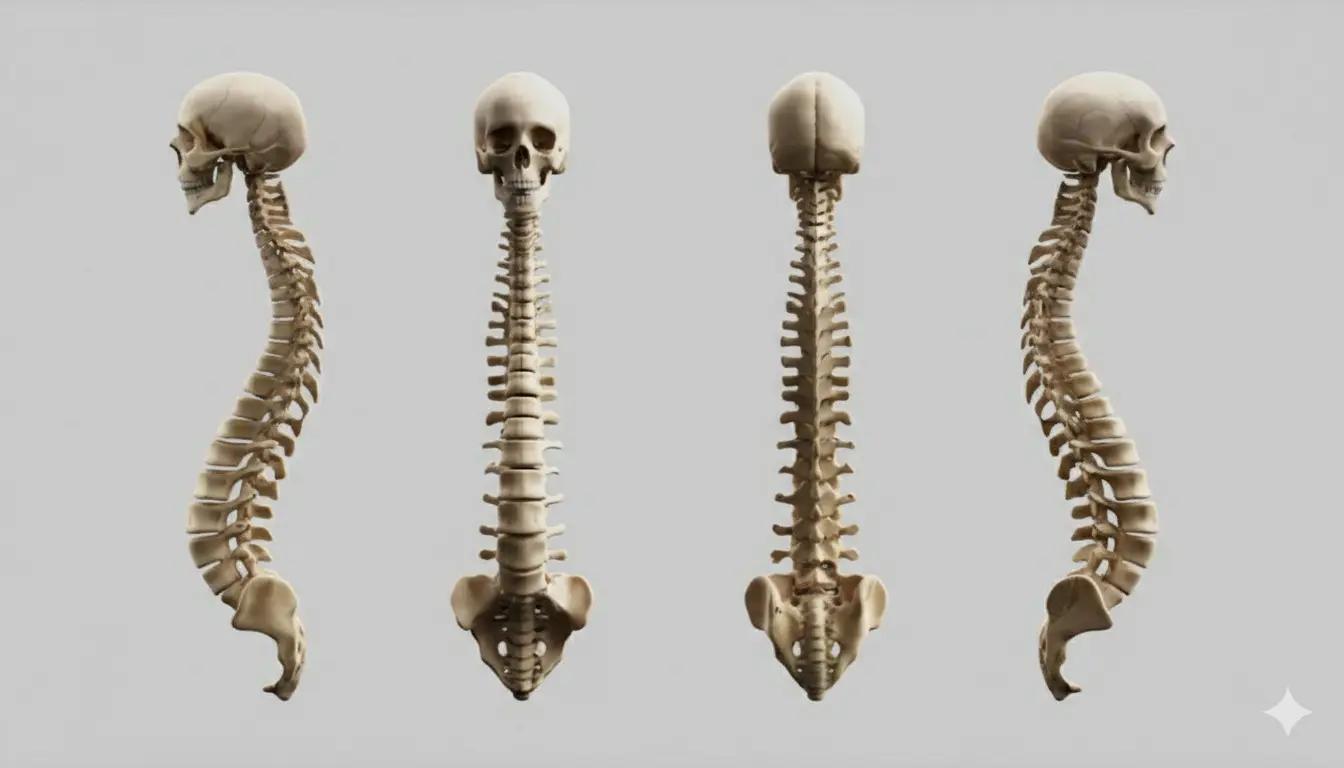
Scans show structure, but they do not show how your body moves, loads, or adapts.
A thorough clinical assessment helps identify what is actually driving your pain and ensures treatment is directed at the true source rather than an incidental finding.
Quick Tip: Before requesting a scan, consider booking a clinical assessment first. Our chiropractors and physiotherapists can determine whether imaging would genuinely change your treatment plan.
What to Remember
Scans can be extremely useful in the right situations, but they should not replace clinical reasoning. Accurate assessment is vital to ensure the correct treatment, particularly when scan findings and symptoms do not match.
If you’re experiencing back, neck, or joint pain and wondering whether you need a scan, our team at Costa Health can help you understand the best next steps for your specific situation.
Contact us today https://costahealth.es/contact/
Frequently Asked Questions
Do most people with pain need a scan?
No. Most musculoskeletal pain can be assessed and managed effectively without imaging. A thorough clinical examination often provides more useful information than a scan.
Can a scan show the exact cause of my pain?
Not always. Many findings on scans are incidental and unrelated to your symptoms. A scan shows structure, not function, which is why clinical assessment remains essential.
Are disc herniations always painful?
No. Studies show that many people have disc herniations without experiencing any pain. The presence of a herniation on a scan does not automatically mean it is causing your symptoms.
Should I worry if my scan shows a disc prolapse?
Not necessarily. Scan findings need to be interpreted alongside your symptoms and physical examination. Many disc prolapses are incidental and not the source of pain.
Can pain come from somewhere other than where it’s felt?
Yes. Movement patterns and muscle overload can refer pain to other areas of the body. This is why a comprehensive assessment of how you move is so important.
Will treatment still help if I don’t address the scan finding?
Yes, if treatment targets the true driver of your pain. Treating the actual cause of symptoms often produces better results than focusing on incidental scan findings.
When should imaging definitely be considered?
After significant trauma, when you have worsening neurological symptoms such as progressive weakness or numbness, or when there are other red flags that need to be ruled out.
Why is clinical assessment so important?
Clinical assessment ensures treatment is based on how your body actually functions, not just what appears on a scan. It identifies the true source of your pain and guides effective treatment.